The Logistics Challenges of Home Delivery For Hospital Pharmacies – Issues And Solutions

Blog > Home healthcare > The Logistics Challenges of Home Delivery For Hospital Pharmacies – Issues And Solutions
The Logistics Challenges of Home Delivery For Hospital Pharmacies – Issues And Solutions
Published on 16 May 2024 • Reading time: 8 min read
Home care is becoming increasingly important for the well-being of patients. It enables them to return to their own homes, while continuing to benefit from very vital care. However, it requires an efficient supply of medicines, to avoid any interruption in care or medical error.
These logistics are largely handled by hospital pharmacies. These healthcare professionals are faced with numerous safety issues, such as the need for traceability, data transmission, therapeutic adaptation and compliance with dosage requirements. At the same time, they need to optimise their costs, ensure real-time deliveries and avoid drug shortages.
To help you find your way through this maze of issues, we take a look in this article at:
- The current management of medicines for patients hospitalised at home
- The logistics challenges of home delivery for hospital pharmacies
- New technologies to meet the challenges of healthcare logistics
The delivery of medicines is crucial for patients hospitalised at home. This service guarantees the continuity of medical treatment. Technological solutions enable hospital pharmacies to simplify these healthcare logistics.
Who manages the delivery of medicines to homecare patients?
Homecare Services are authorised within a comprehensive framework. Admission to home care requires a medical prescription and the explicit agreement of the patient or their representative, as well as the attending GP. In the absence of these authorisations or of an available Homecare Services structure, patients are kept in hospital. The treatments prescribed at home vary considerably. They may consist of capsules or tablets administered orally. But there are also more complex treatments, involving injectable solutions via intravenous infusion. Only certain organisations can offer this type of care at home.
Authorised home care facilities are considered as hospital establishments without accommodation. They are subject to the same constraints as private and public hospitals. Among their obligations, they must supply medicines under the conditions set by the legal framework. To do this, they rely on their in-house pharmacies. If there is no such facility, they are also authorised to sign an agreement with a pharmacist managing another hospital pharmacy or with the manager of a dispensing pharmacy.
Hospital pharmacies manage, supply, prepare, control, evaluate and dispense the medicines and health products required by home care patients. They also ensure that patients are kept informed and that medicines are used correctly, in collaboration with the care team.

The pharmacist in charge of hospital pharmacies organises the dispensing of prescribed medicines.
The pharmacist in charge of a hospital pharmacy receives all the prescriptions dispensed by the Homecare Services facility for nursing care at home. In agreement with the coordinating doctor, he organises the dispensing circuit for each patient for the prescribed medicines (oral or intravenous) or any other medical devices. They may also use dispensing pharmacies, in addition to products from their in-house pharmacy.
What are the logistics challenges involved in delivering hospitalised patients to their homes?
We have identified 3 main types of logistics challenge for home delivery of medicines from hospital pharmacies.

The three logistics challenges involved in delivering medicines to homecare patients.
1. Securing and decommissioning medicines (serialisation)
The first challenge is common to the overall management of medical treatments, namely the need for traceability and security of medicines and other medical devices.
It meets the need for regulatory compliance and control of good manufacturing practice by the health authorities. This includes compliance with storage, distribution and documentation standards. The aim is to ensure the quality and safety of care, as well as the confidentiality of patient data.
In addition, it must be possible to trace each treatment from the moment it is acquired to the moment it is administered to the patient. This includes managing medication reminders and monitoring side effects. It requires genuine monitoring and expertise in medicines, in coordination with the healthcare team.
The traceability of medicines also helps to prevent the risk of falsification. This risk has increased since the Covid-19 pandemic and the development of e-commerce. To tackle this problem, the European Parliament has introduced two new types of system: serialisation and tamper evident testing of medicine boxes.
Serialisation has been gradually introduced in hospitals since 2019. It requires a unique identifier to be affixed to each box. This number is recorded in a central database. It is scanned when the medicine is dispensed to verify its authenticity.
Implementing serialisation involves major technical, organisational and IT changes for pharmacies.
The decommissioning of medicine boxes (deactivation of the unique identifier) involves additional work for hospital pharmacies. They can decommission, scan and repackage the drugs when they are received, restocked or distributed. However, this time-consuming activity requires additional space and resources. In particular, the reception software needs to be interfaced with the national database. Investment in human resources, scanners and computer software is therefore necessary.
The challenges facing hospital pharmacists do not stop there. They also have to manage the return of products from other departments or establishments, as well as other non-serialised products in stock.

The serialisation of medicines is progressively being introduced in hospitals.
2. Transfer of data and responsibility between healthcare professionals
This problem is added to the safety issues. From the prescriber to the patient, via the pharmacist, the administrative departments, the carrier and the care team: the distribution chain is very long.
The challenge begins as soon as the prescription is handed in. Hospital software and Homecare Services tools are rarely connected. This prevents the direct transfer of data in structured format (name of treatment, dosage and frequency of administration). Over 80% of Homecare Services structures have to re-enter prescriptions into their software. This is both time-consuming and a source of transcription and medication errors.
The numerous intermediaries also create risks for therapeutic compliance and compliance with protocols. To put it more clearly, the lack of direct contact between the doctor, the patient and the hospital pharmacist can be detrimental to the proper administration of medical treatments.
The same applies to any side effects or other drug interactions. They require very good coordination between the hospital team and the carers at home, to carry out the necessary clinical monitoring, adjust doses and react quickly if necessary.
3. Optimised and secure stocks for guaranteed deliveries in real time
The obligations of hospital pharmacists are not limited to securing medicines and correctly transcribing prescriptions. They must also ensure that they have sufficient stocks of oral tablets, injectable solutions, vaccines, personal protective equipment (PPE), hygiene products and other medical devices.
And this 7 days a week, as the care of people hospitalised in hospitals or at home does not stop at weekends. Any delay in providing care or taking medication can have a serious impact on their state of health.
This obligation is all the more critical given the increasing number of drug shortages in recent years. In 2023, 1,634 drug references were reported as being out of stock or in short supply in the UK. Hospital pharmacies need to be on the alert and hold sufficient stocks.
Despite these major constraints, hospital pharmacies need to guarantee reliable supplies in real time, while optimising costs and delivery times.
Good stock management and control are essential. They enable automated replenishment before a critical stock threshold is reached.
Good monitoring of logistics flows also helps to anticipate future needs, seasonal peaks, frequencies, trends and future requirements for medical treatments, depending on the areas in which the hospitals concerned operate.
And optimising deliveries ensures that patients receive their supplies in real time, without any delay in receiving care in their own homes.
What technological solutions are needed to meet these healthcare logistics challenges?
Numerous technological solutions have been developed in recent years to help hospital pharmacies and other healthcare services meet these safety, management and optimisation challenges.
We won’t be able to list them all in this article. But we’d like to take a look at some of the most innovative and effective.

The technological solutions available to meet the challenges of healthcare logistics.
1. Automated transfer of prescription data to homecare services software
MHComm has tackled the problem of transferring prescriptions into Homecare Services software. It has integrated automated transcription technology of Posos into the MHCare computerised patient record, which specialises in homecare treatment. This partnership represents a significant step forward. When patients are admitted to homecare, Posos enables treatments and dosages to be transcribed instantly from paper prescriptions, simply by taking a photograph of the prescription. The result is fewer transcription errors, time saved for carers and greater safety for patients.
2. Improved picking through automation and assisted reality
Whether it’s for people treated in hospital or at home, the preparation of medical treatments requires both accuracy and speed. Pharmacists and nursing staff have to follow prescriptions literally, despite the large number of references available and time constraints.
The use of automated hospital trolleys can improve the efficiency and safety of drug distribution, from the central pharmacy to the patient. This is particularly true of the innovative system Cart from Antares Vision Group. Once the patient has been identified, the prescription is displayed on screen. The robotic system included in the trolley then places the medication directly on the work surface. The result: guaranteed time savings, no constraints on staff, and added safety in the supply of medicines.
The adoption of assisted reality technologies also improves accuracy and reduces errors in the dispensing of medicines. The Citadelle hospital in Liège is currently experimenting with glasses connected to a small keyboard (a keypad) attached to the arm or belt. This system, invented by the start-up Get Your Way, replaces paper distribution lists. It considerably reduces the need for checks and the risk of errors during preparation. In practice, the Keypad is linked by WiFi to the server that hosts the distribution lists. The information contained in the lists is sent to the preparation technician’s or pharmacist’s glasses. All that’s left for them to do is read it and check the medicines they have taken using the built-in RFID tag reader.
3. Optimising deliveries with route optimisation software
Once prepared, medicines need to be delivered quickly so that they can be administered on time. However, it is not feasible to drop off medicines in front of patients’ homes. Hospital pharmacies therefore need to be able to schedule suitable delivery times and slots, while avoiding the need for delivery staff to work overtime. Not to mention last-minute tasks and urgent changes to prescriptions. When patients are hospitalised at home, the delivery of medicines is often a vital necessity, which means there can be no delays. It requires real organisation, which is difficult to achieve manually.
Like GHEMM, hospital group of Grand Est, France, it is possible to opt for route optimisation software, such as the one from AntsRoute, to simplify the planning of deliveries to people receiving care at home.
It enables:
- Automatically plan visits.
- Optimise itineraries and reduce the number of kilometres travelled.
- Take into account the constraints of patients, caregivers and delivery staff.
- Schedule appointments.
- Ensure traceability of deliveries.
Plus many other optimisation options available on request.
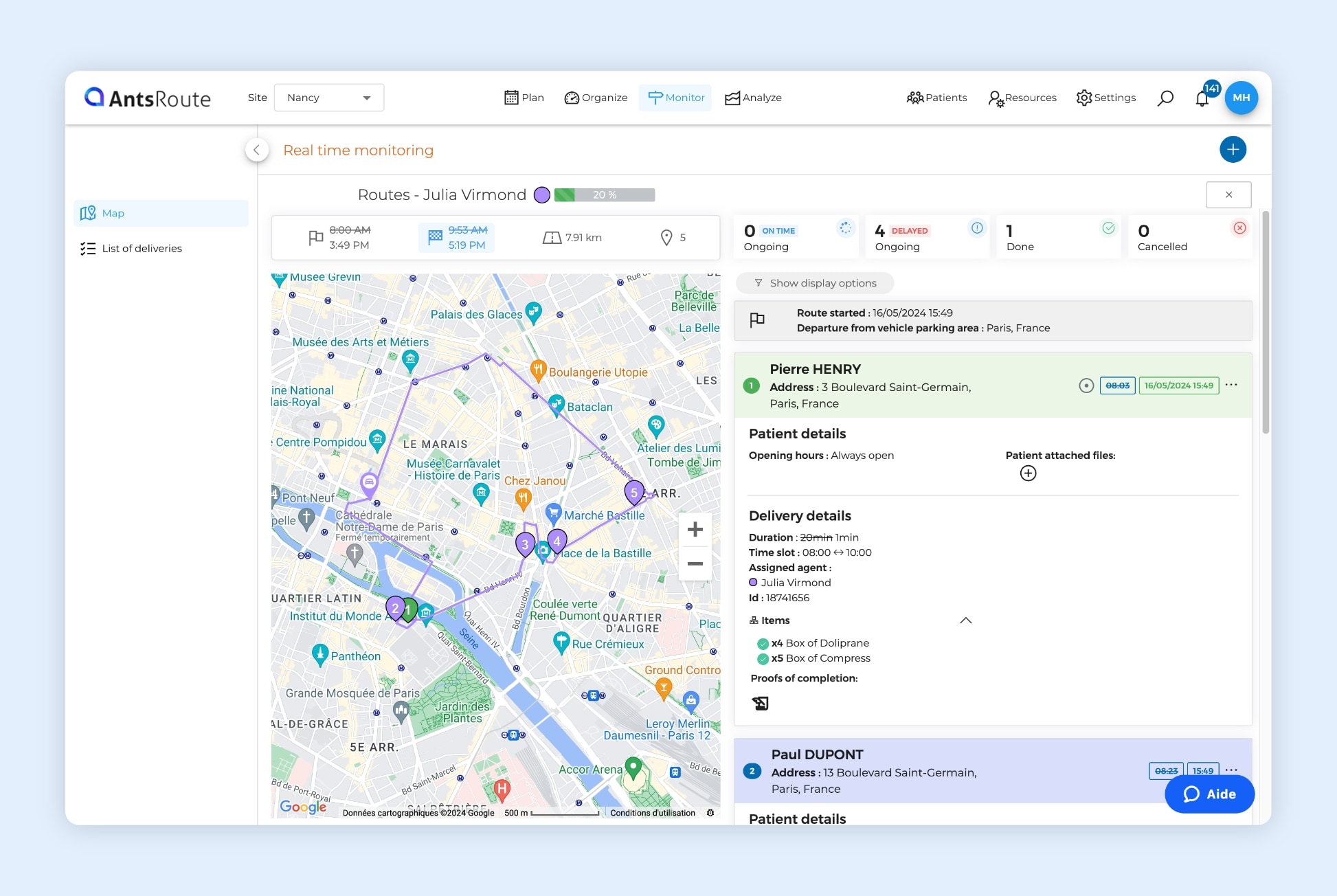
The optimisation of a delivery route on AntsRoute.
Thanks to the AntsRoute software, the logistics department at GHEMM is able to build secure routes in 5 to 10 minutes, instead of the hour it used to take. In particular, the software has enabled it to optimise routes and automatically integrate transit times of 15 minutes for each patient. The result: significant time savings, secure deliveries, respect for working hours and reassured patients.
There are many issues, but solutions are available to further develop homecare services in complete safety.
Free 7-day trial | No credit card required
Contenu
- Who manages the delivery of medicines to homecare patients?
- What are the logistics challenges involved in delivering hospitalised patients to their homes?
- 1. Securing and decommissioning medicines (serialisation)
- 2. Transfer of data and responsibility between healthcare professionals
- 3. Optimised and secure stocks for guaranteed deliveries in real time
- What technological solutions are needed to meet these healthcare logistics challenges?
- 1. Automated transfer of prescription data to homecare services software
- 2. Improved picking through automation and assisted reality
- 3. Optimising deliveries with route optimisation software